Latest articles:
What is a Consolidated Invoice and How It Works?
Consolidated invoicing explained: what is a consolidated invoice, why employers consolidate benefit plan invoices, and how it simplifies billing.

February 26, 2026
What Is Consolidated Billing? Benefits & Best Practices
Learn how consolidated billing for employee benefit plans works, how it differs from traditional billing, and why it matters.

February 17, 2026
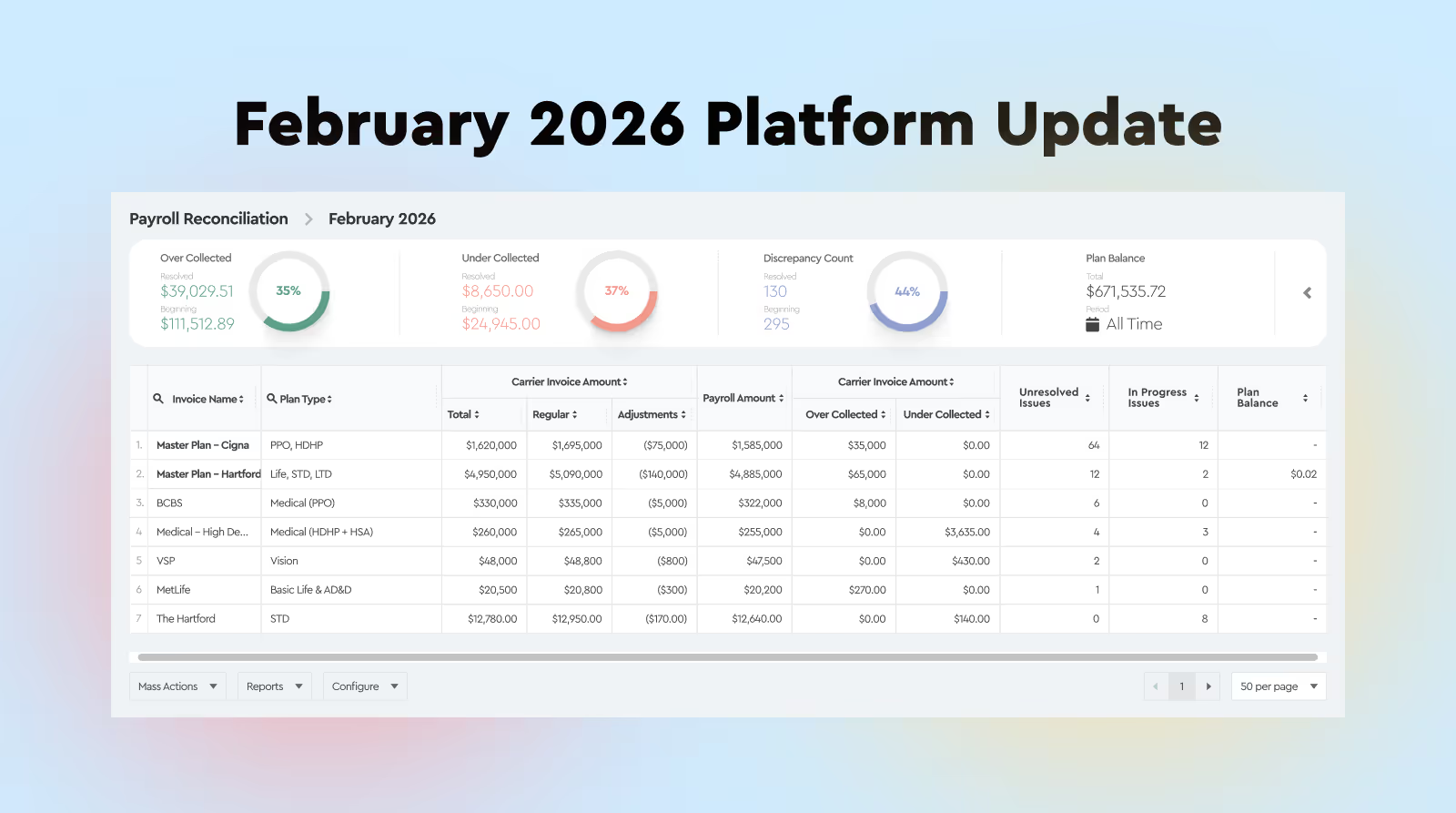
February 2026 Platform Update
February platform update with improvements to benefits reconciliation, pre-pay invoice matching, variance tracking, notes visibility, and consolidated

February 4, 2026