Ashley Ball
Director of Trust Operations



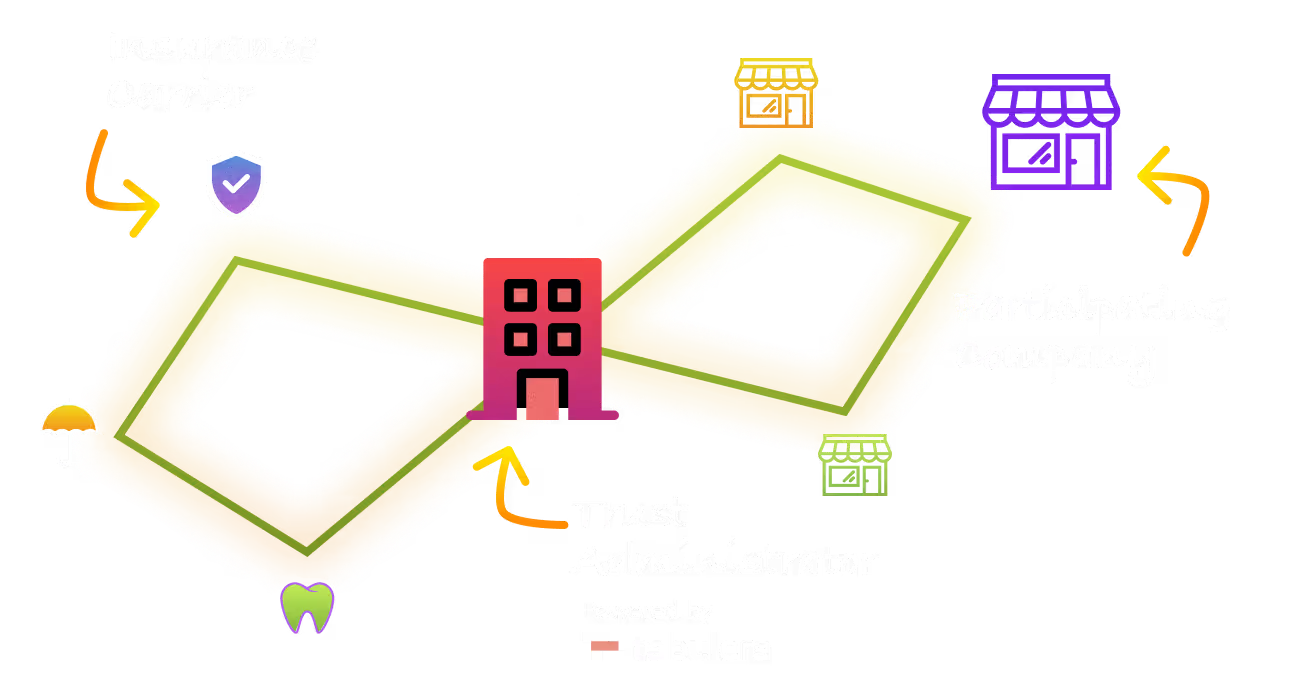
“Tabulera revolutionized premium administration for Trusts with automated invoicing and seamless payment processing, resulting in smoother and more efficient operations.”
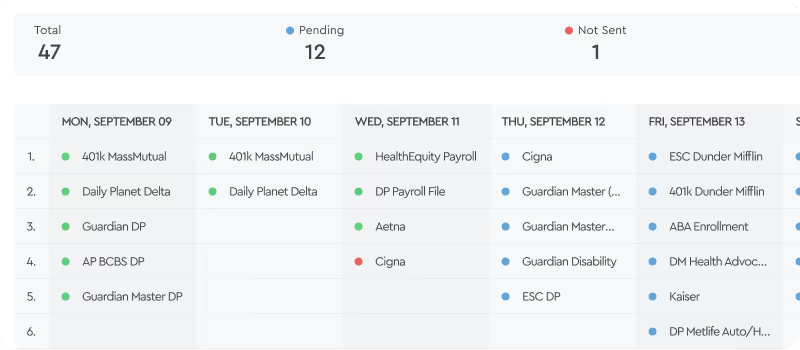
100+
Participating Employers
20+
Invoices
per Month
10+
eDI
Feeds