October 22, 2024
Turning Additional Services into Agency Revenue
This article should be valuable to brokers and agencies that want to expand their services without overwhelming their teams. We explore how to effectively offer premium administration services, specifically benefit invoice audits, streamline auditing operations, and meet your clients' growing needs.
Introduction
In today's dynamic benefits landscape, brokers are continually seeking ways to enhance their service offerings and generate new revenue streams. One area gaining significant traction is premium administration services. As employers grapple with the complexities of benefits billing, invoice audits, and carrier payments, brokers have a unique opportunity to step in and provide valuable solutions. However, offering these services comes with its own set of challenges, especially when service teams are stretched thin.
The Competitive Landscape and Evolving Role of Benefit Brokers
Benefit brokers have traditionally served as intermediaries between employers and insurance carriers, helping businesses select the best benefits packages for their employees. However, the role is expanding. For instance, Professional Employer Organizations (PEOs), Association Health Plans and other group benefit arrangements offer a myriad of overlapping services including purchasing, reconciliation and payment of plan premiums.
Small to mid-sized employers now look to service providers not just for plan selection but also for assistance with administrative tasks that accompany those plans. This shift presents both an opportunity and a challenge: brokers can increase their revenue by offering additional services, but they must also manage the operational demands these services entail.
Understanding Premium Administration Services
What Is Premium Administration?
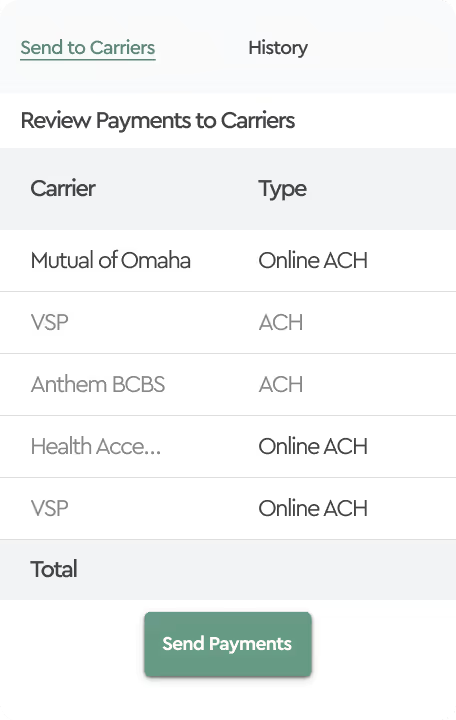
Premium administration involves managing the processes related to benefits billing, including auditing invoices and ensuring accurate carrier payments. By handling these complex tasks, it relieves the employer's HR and benefits teams of administrative burdens that sometimes have more to do with accounting rather than benefits.
For employers, streamlined premium administration means fewer errors, reduced overpayments, and compliance assurance. For brokers, it opens up a new revenue stream and strengthens client relationships by providing a comprehensive service package.
Two Ways Brokers Can Assist with Premium Administration
There are two ways brokers can help clients with their premium administration needs and generate revenue.
Option 1: Providing invoice audit as a service
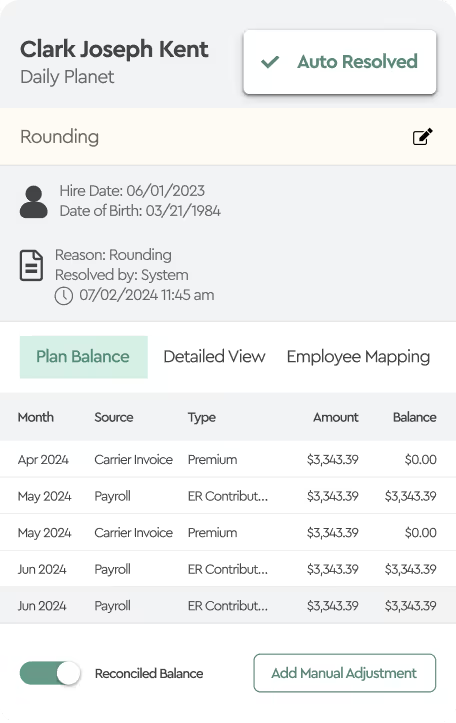
Brokers already have access to their clients' enrollment data through systems like Employee Navigator or other HR software. This means they can offer benefits reconciliation services by using this data to audit invoices effectively. By comparing the enrollment information with carrier invoices, brokers can spot discrepancies including incorrect charges or coverage errors, which can happen as a result of human error or system misconfiguration on both, employer and insurance carrier sides.
Challenges of Manual Invoice Auditing
Manual invoice auditing, though seemingly straightforward, is labor-intensive and requires meticulous attention to detail. Brokers often lack staff with both accounting and benefits expertise, making the process inefficient and prone to errors.
These challenges become even more significant when working with clients who have complex company structures, multiple HR systems, and multiple locations. Sometimes, clients grow through mergers and acquisitions, bringing in subsidiaries that use different HR systems than the parent company. This adds layers of complexity to the auditing process. Brokers can assist these clients by figuring out exactly how much each location or business unit owes for their benefit plans. By bringing together and matching data from different systems, brokers help organizations handle this added complexity, ensuring billing is accurate and costs are correctly allocated throughout the entire company. However, doing this manually increases the risk of mistakes and can overwhelm service teams.
Case Study: Uncovering Invoice Discrepancies
A broker auditing invoices for multiple clients with 5,000 employees (avg.) on benefits and 128 invoices revealed significant discrepancies:
- 84% of plan participants automatically matched between the carrier invoices and the enrollment data.
Of the remaining 16% the following was observed:
- 2% had a Tier Mismatch, where coverage levels differed (e.g., "Employee Only" vs. "Employee + Spouse").
- 17.5% showed a Rate Mismatch, indicating discrepancies between invoiced amounts and expected amounts.
- 33.5% involved Timing Differences due to Suspected Termination, where terminated employees were still on invoices.
- 35.5% had Timing Differences due to Suspected New Hires, with new employees not yet appearing on invoices.
While some discrepancies would resolve in subsequent billing cycles, issues like tier and rate mismatches could lead to financial losses or legal complications if left unaddressed. Auditing all employees and invoices manually each month is not sustainable, highlighting the need for streamlined processes.
Option 2: Winning Large Deals with Limited Resources
Securing large contracts often involves responding to Requests for Proposals (RFPs), where employers outline their specific needs and expectations. These proposals require brokers to meet complex requirements and offer supporting service packages, which often include premium administration services.
For brokers, especially smaller ones or those without extensive administrative teams, meeting these demands can be challenging. Without the necessary infrastructure, competing for large deals can strain existing resources and make it tough to match larger firms with more substantial teams and systems.
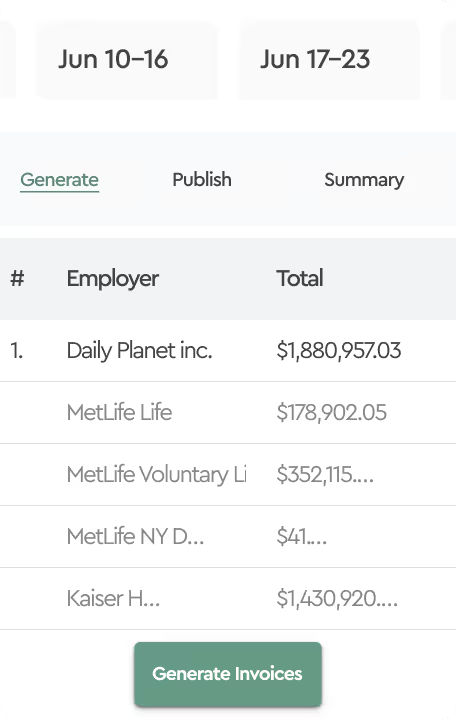
An effective strategy is for brokers to partner with technology providers to bundle insurance offerings with software solutions. This approach allows brokers to provide tools that enable their service teams to handle benefit plan billing more efficiently. As a result, the agency can assist employer's HR and benefits teams to manage complex billing tasks across multiple locations or different HR systems, especially after mergers and acquisitions. Bundling these services gives employers a single solution to simplify benefit plan billing operations and improve efficiency, while brokers add value without overextending their resources.
The Importance of Invoice Auditing
Common Discrepancies and Their Impacts
Invoice discrepancies are not just administrative nuisances; they have real financial and legal implications. Overpaying premiums affects an employer's bottom line, while underpayments or coverage gaps can lead to compliance issues and employee dissatisfaction.
Financial and Legal Risks
Failing to identify and correct invoice errors can result in:
- Financial Losses: Paying for coverage not received or for terminated employees.
- Compliance Issues: Non-adherence to regulations like COBRA can lead to penalties.
- Employee Relations Problems: Employees may face coverage gaps, leading to mistrust and potential legal action.
Conclusion
Premium administration services represent a significant opportunity for benefit plan brokers and agencies to expand their offerings and strengthen client relationships. Whether by providing these services directly or by enabling clients through technology solutions, enable brokers to compete in the market and navigate the challenges of efficiency and resource management. Embracing technological tools and partnerships can help brokers deliver these services in a repeatable and high-quality offering without overburdening their teams.
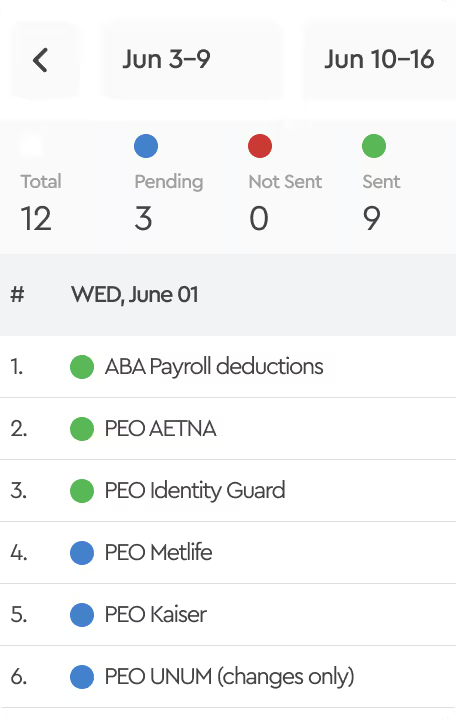
How Tabulera Fits In
Tabulera offers a platform that seamlessly integrates with enrollment systems like Employee Navigator, isolved and other HRIS platforms enabling brokers to efficiently audit client invoices. With smart algorithms and configurable settings, Tabulera's benefits reconciliation module automates much of the auditing process. It filters out employees without discrepancies, highlights timing, rate, or tier differences, and aggregates benefits-related data in one place for easier research of the underlying issue. This allows brokers to focus on resolving genuine issues, significantly reducing the administrative burden. By partnering with Tabulera, brokers can enhance their service offerings, win larger deals, and provide clients with the tools they need for effective premium administration.