How a Benefits Agency reduced the invoice audit effort by 84%
Tabulera allows brokerages to offer Benefits Invoice Audit as a Service without overloading their workforce
The Problem
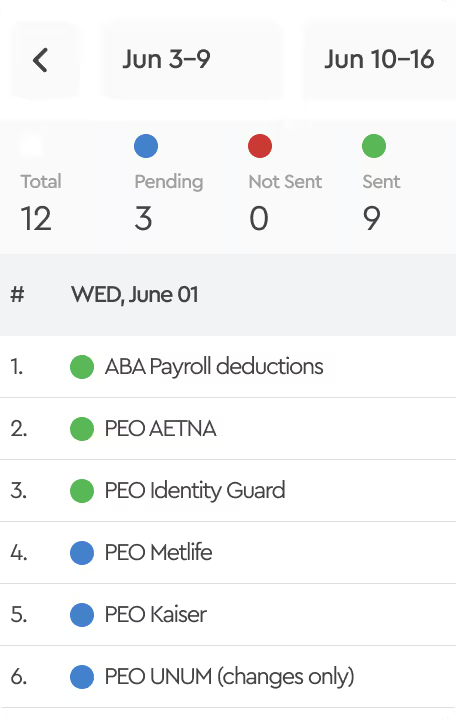
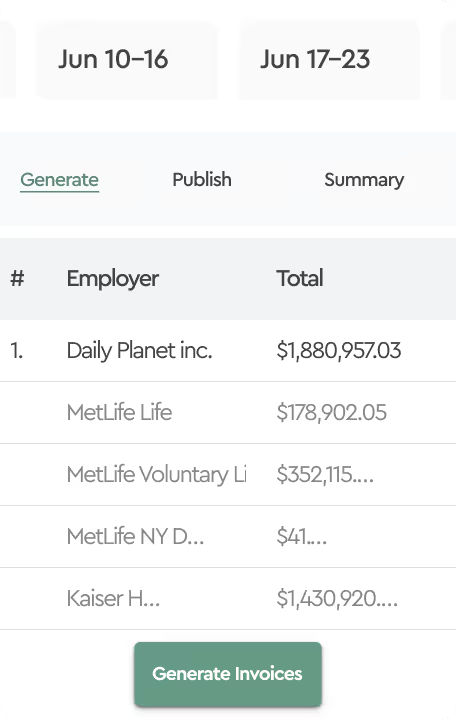
Our brokerage clients faced a common challenge in managing benefit invoice audits (also known as benefits reconciliation) for their employer groups. With an average of 4 list-bill invoices per employer against enrollment data from Employee Navigator and other benefits administration systems, reconciliation was a time-consuming task.
Moreover, the reconciliation of COBRA invoice transactions against COBRA Enrollment data required meticulous attention to detail to prevent errors and financial losses for their clients.
Most brokers lack a dedicated team of benefits reconciliation specialists and rely on account managers to provide this service. The historical manual processes in Excel lacked scalability and auditability.
The Solution
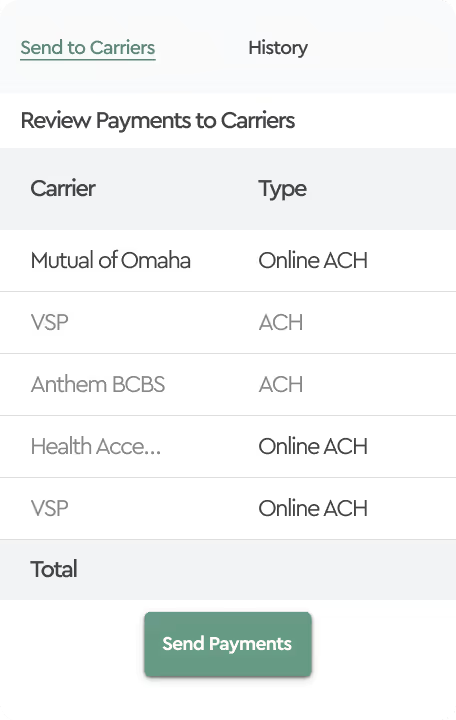
Tabulera's Benefits Reconciliation Module provided an efficient solution to automate the benefits invoice audit process. By configuring the module for Enrollment Reconciliation, brokers could seamlessly match enrollment data from Employee Navigator and other HRIS with list-bill invoices.

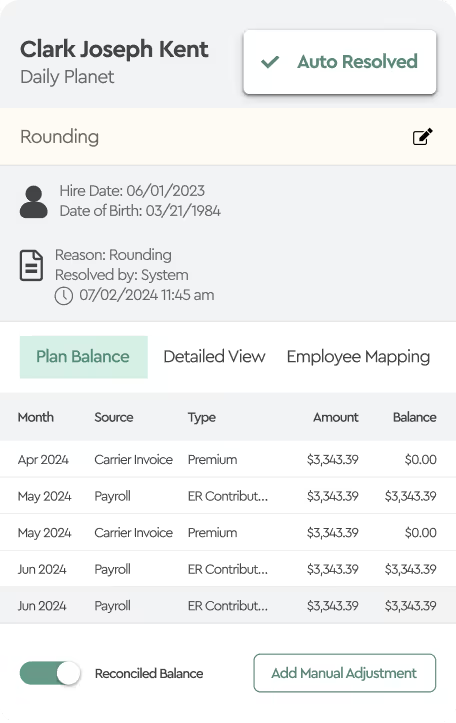
This indicates that the system automatically identified 84% of employees from the enrollment file within the carrier invoice, cross-referenced the amounts and tier coverages, and ensured consistency between both sources. Moreover, employees with rounding variances were also automatically resolved.
The majority of the remaining 16% of variances consisted of:
- 2% Tier Mismatch
Different coverage levels between the invoice and the enrollment system (e.g., “Employee only” vs. “Employee + Spouse”). - 17.5% Rate Mismatch
Discrepancy between the invoiced amount and expected amount in the enrollment data. - 33.5 % Timing difference due to suspected termination*
Employee terminated in the system but still present on the invoice. - 35.5% Timing difference due to suspected new hires*
Employee not on the invoice but present in the enrollment file, likely due to a new hire after invoice generation.
*Both discrepancies due to timing differences were often automatically resolved in subsequent invoices, reflecting timing differences such as new hires or terminations post-invoice generation.
The Conclusion
Since implementing Tabulera's Benefits Reconciliation Module, brokers have experienced significant improvements in the audit of benefit invoices. Over the last three months, the system has consistently achieved an impressive average auto-match rate of 84%.
Manual root cause analysis only needed to be performed for 16% of employees with billing variances, primarily involving timing issues and plan mismatches.
With newfound efficiency, brokers can now offer benefits reconciliation services to every client without substantial workforce expansion, ensuring seamless scalability.