Transforming Benefit Invoice Audits Through Agency Partnerships
In the competitive landscape of Agencies, achieving efficiency and accuracy in premium administration is paramount.
This case study explores how Agencies that identify a client need to automate their benefit invoice audit and reconciliation process play a critical role in their clients' success.
Client Background
Our client, a large, multi-state organization in the retail and energy sectors, operates numerous convenience stores, heating oil offices, and service stations, and serves hundreds of gasoline dealers across several states.
They were in search of a consolidated billing and benefits reconciliation solution.
The organization employs approximately 600 benefit-eligible employees, but their benefits administration team consists of just one person, underscoring the need for an efficient, automated system.
The Problem
Managing benefits billing for 600 employees with a single team member is a daunting task. The client needed a solution to streamline the benefit invoice audits to reduce manual workload and minimize errors and found Tabulera’s Benefits Reconciliation Module to be the cornerstone.
The Solution
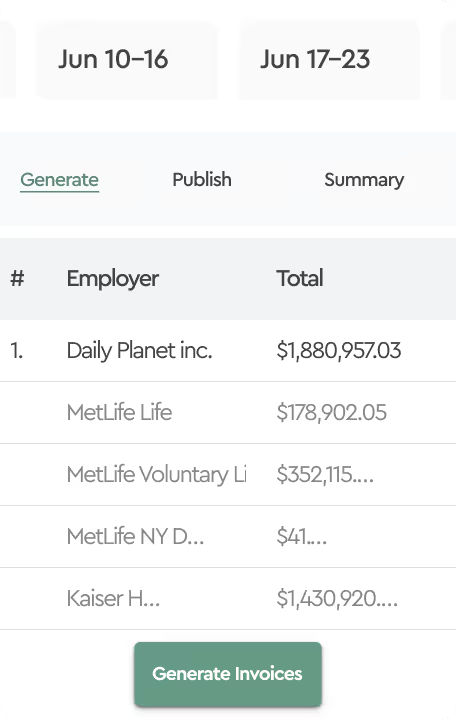
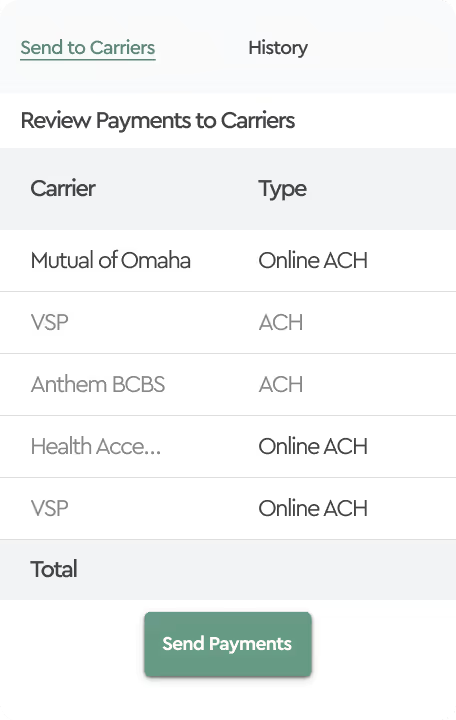
After reviewing the client requirements with the Agency and an initial client meeting, it was agreed to implement three Tabulera modules to address their billing needs, with Benefits Reconciliation leading the way.
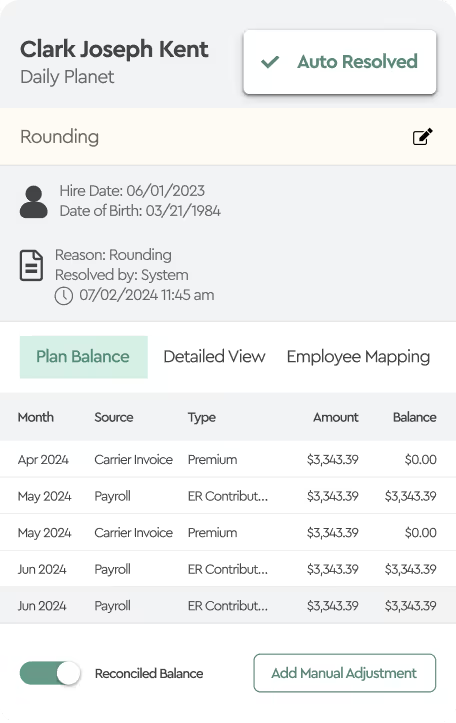
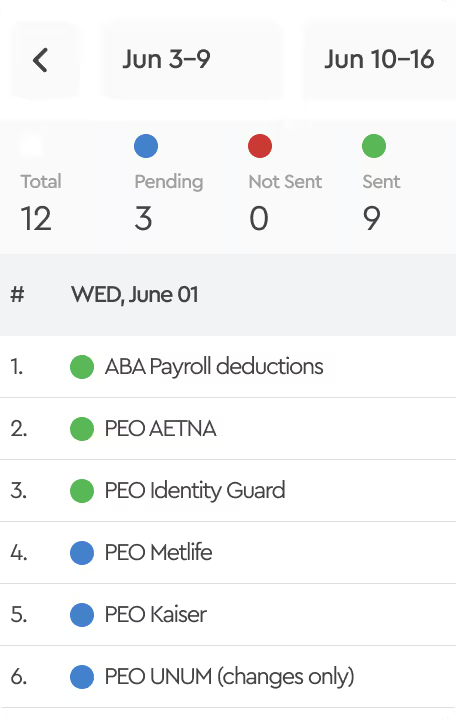
Benefits Reconciliation Module: The module was implemented to identify benefit invoice discrepancies by automating the comparison of payroll data with carrier invoices. It ensures discrepancies are identified and resolved efficiently, significantly reducing manual effort and minimizing errors.
These solutions together streamlined the client’s benefits billing and reconciliation processes, allowing their small team to manage the extensive operations more effectively.
The Results
Since the implementation of Tabulera’s Benefits Reconciliation Module, the client has achieved remarkable results:

91% Auto Resolution Rate
The system successfully resolved the vast majority of invoice line items, significantly reducing the manual effort required.
Remaining Discrepancies: The benefits team limited their review to only 8% of employees. These discrepancies were categorized as follows:

60% Rate Differential
These discrepancies can lead to overpayments to insurance carriers and under-collections from employee deductions, which can create serious financial and compliance consequences.
35% Terminations in Transit
These discrepancies involved employees listed on the carrier invoice but missing from the payroll system.
5% Enrollments in Transit
These discrepancies involved employees listed on the payroll system but missing from the carrier invoice.
The Impact
The implementation of the Benefits Reconciliation Module has had a profound impact on the client’s operations. The high auto-resolution rate has freed up significant time for the benefits administration team, allowing the single team member to focus on more strategic tasks rather than being bogged down by hunting for discrepancies one by one.
The system’s ability to accurately identify and categorize discrepancies has also improved financial accuracy and control, reducing the risk of overpayments and ensuring that all payroll deductions and employer contributions are correctly matched with carrier invoices.
Conclusion
This case study demonstrates the power of leveraging agency referrals to connect clients with the right third-party solutions. Agencies play a critical role, not just as intermediaries but also as enablers of their clients' transformation of benefits premium administration processes, achieving greater efficiency and accuracy.
The Benefits Reconciliation Module has proven to be an invaluable tool for performing benefit invoice audits, providing a scalable solution that meets the needs of organizations with limited administrative resources.
If your agency is looking to streamline its benefits invoice audit process, consider how advanced solutions can help them achieve similar success. Contact us today to learn more about our offerings and how we can support your needs.