August 19, 2025
Streamlining Benefits Enrollment with EDI 834
With proper planning and implementation, the EDI 834 file format can be a game-changer for benefits enrollment, bringing speed, accuracy, and simplicity to a complex process. This article explains what an EDI 834 enrollment file is, how it works, its structure, implementation considerations, and best practices for using it to streamline enrollment.
What is EDI 834?
EDI 834 (ANSI X12 834) is an electronic file format designated for transmitting health plan enrollment and maintenance data. It’s officially known as the Benefit Enrollment and Maintenance transaction set. In simple terms, an EDI 834 file allows employers or other plan sponsors to exchange enrollment information about employees (and their dependents) with health insurance carriers in a standardized way. The format was introduced under HIPAA requirements – HIPAA 5010 standards mandate that all health plans must accept the ANSI 834 version 5010 format for electronic enrollments.
An 834 enrollment file typically flows from the “plan sponsor” of the insurance (an employer, PEO, union, or association) to the “payer” (e.g. insurance company or HMO/PPO). For example, a company (as plan sponsor) will send an EDI 834 file to its insurance carrier to add a new hire to the health plan or update an employee’s coverage. This standardized file replaces the need for paper forms or manual web portal entries by moving the data directly between systems (HR/payroll systems to insurance systems) in a consistent format.
Who uses EDI 834?
A variety of organizations in the benefits space use 834 files for enrollment processing. Common senders include employers (or their HR/benefits systems) and third-party benefit administrators, while receivers are typically insurance carriers or health plan providers. Government health programs like Medicaid/Medicare also use EDI 834 to manage enrollment in public plans. In practice, this transaction set is used to handle actions such as:
New Enrollments: Adding a new subscriber (employee) and their dependents to a health plan.
Changes to Enrollment: Updating a member’s information or coverage (for instance, changing plan options or correcting data).
Reinstatements: Re-activating a lapsed or terminated enrollment for a member.
Terminations: Removing a member from coverage (e.g. when an employee leaves the company or a dependent ages out).
In essence, the EDI 834 file covers the full lifecycle of enrollment events from initial sign-ups to changes and cancellations – ensuring all parties maintain synchronized records of who is covered under a health plan.
What Information is in an 834 Enrollment File?
An 834 file is a structured text file containing many data elements that together convey the enrollment details. Each data element represents a specific fact about a member or the enrollment. For example, there are elements for a subscriber’s name, address, date of birth, plan selection, effective dates, etc.. A typical 834 enrollment file will include information such as:
- Subscriber Personal Info: Name of the employee or policy subscriber and an identifying number (such as a member ID or Social Security Number).
- Dependent Info: If dependents (spouse, children) are covered, their names and related details are included (often tied to the subscriber’s record).
- Plan and Coverage Details: The health plan or benefit plan identifiers, such as plan codes or network identifiers, indicating which plan the person is enrolling in.
- Enrollment Dates: Important dates like the coverage effective date, and possibly coverage end date if applicable.
- Eligibility and Status: Information about the member’s eligibility or any specific benefit information, as well as indicators of the action being taken (e.g. new enrollment vs. change).
All this data is encoded in the 834 file as segments of text separated by special delimiters (like asterisks * between data elements and tildes ~ marking the end of segments). Because the 834 format is standardized, each piece of information appears in a predetermined sequence, making it possible for the receiver’s system to interpret the data correctly.
Notably, whenever an enrollment file (834) is sent, the receiver will return a 999 Implementation Acknowledgment to confirm that the file was received and whether it was accepted or had any errors. The 999 acknowledgment is an automatic response that indicates if the 834 file’s structure was valid and successfully processed. (If the 834 file fails compliance checks, the 999 will report rejection or errors, which then need to be addressed by the sender.)
[[Note]]
Aside: While EDI 834 is a widely adopted standard for enrollment data, some carriers or vendors may use alternative formats if an EDI link is not in place. For instance, enrollment data might sometimes be exchanged via custom CSV files, XML files, or even API/web services in lieu of a standard 834. However, using the ANSI 834 format is generally preferred in the healthcare industry because it adheres to a common standard that all parties recognize, thus reducing miscommunication.
[[/Note]]
EDI 834 File Format and Structure
ANSI X12 834 files have a specific hierarchical structure defined by the X12 standard. At a high level, the file is organized into envelopes and records: an interchange envelope (ISA/IEA segments) wraps one or more functional group envelopes (GS/GE segments), which in turn contain the actual 834 transaction sets (ST/SE segments). Within the 834 transaction, data is grouped into logical sections often referred to as loops. Key loops in an 834 file include the header loop (often loop 1000) for information about the trading partners, a detail loop for each subscriber (loop 2000), and nested loops for related dependent or coverage details (such as loop 2300 for health coverage information).
Each loop contains various segments, which are like rows of data denoted by segment identifiers (e.g., INS, NM1, DTP). Each segment is made up of a sequence of data elements. For example, an INS segment (Insurance member detail) contains several data elements that collectively indicate whether a record is for a subscriber or dependent, the type of action (add, change, terminate), and other coverage status information. A NM1 segment (Name) contains elements for an individual’s last name, first name, middle initial, and an identification number or qualifier.
Key segments commonly found in an EDI 834 file include:
ISA – Interchange Control Header: Appears at the start of the file to identify the sender and receiver of the interchange and set control standards (e.g., delimiters). It contains routing information and control numbers for the entire file transfer.
GS – Functional Group Header: Identifies the type of transaction (in this case, BE for Benefit Enrollment) and groups all related 834 transactions in the file. It also lists sender and receiver codes and a control number.
ST – Transaction Set Header: Indicates the beginning of an individual 834 transaction set within the file (each 834 transaction has its own ST header and SE trailer with matching control numbers).
BGN – Beginning Segment: Conveys the beginning of the transaction information, including a reference code or ID for the enrollment batch and the date/time of the file’s creation. This helps identify the specific enrollment file (for example, a batch number or timestamp).
N1 – Name segments: Provide names of entities. For instance, N1*P5*... gives the plan sponsor name (e.g., the employer), and N1*IN*... gives the insurer name, along with their identification (such as tax ID or other IDs) if required. These segments clarify who the file is from and to.
INS – Member Level Detail: Denotes the start of an individual member’s enrollment record. The INS segment has elements that indicate whether the person is a subscriber or dependent, their relationship code (e.g., 18 for self, 19 for spouse, 01 for subscriber’s spouse in some codes), the type of enrollment action (such as 030 for a new enrollment or change) and coverage status (active, COBRA, etc.). This segment essentially says “here is an enrollment record for a person and here’s what is happening (add/change etc.) with their coverage.”
REF – Reference Information: Appears in various places to carry secondary identifiers. For example, a REF0F segment can carry the subscriber’s policy/account number or member ID assigned by the insurer, and REF1L might carry an alternate ID like a group number or location code. These references help match records in the carrier’s system.
NM1 – Individual Name: Provides the name of the person (subscriber or dependent) and possibly an identifying number qualifier. For a subscriber, it would typically be coded as NM1*IL (insured individual) followed by last name, first name, middle initial, and an identification number such as SSN or an internal member ID (with a qualifier like “34” indicating SSN) in the data elements.
N3/N4 – Address Segments: Give the mailing address of the individual. N3 is the street address (with two data elements allowing street line 1 and line 2), and N4 includes the city, state, ZIP code, and country. These segments appear if address information is being transmitted for the member (often for new enrollments).
DMG – Demographic Information: Contains date of birth, gender, and marital status or other demographic details for the individual. For example, DMGD819800101*M~ indicates a birth date of 01/01/1980 and gender Male. This is important for the insurer’s records of the member or dependent.
HD – Health Coverage: Specifies the details of the health plan coverage that the person is enrolling in. The HD segment can include the coverage level or plan code and coverage type. For instance, it might indicate medical, dental, vision coverage, etc., and the plan or option selected. (In some 834 implementations, multiple HD segments and subordinate segments can appear if the individual has multiple benefits like medical, dental, life insurance, etc., each in a separate loop.)
DTP – Date/Time Reference: Used to convey dates related to the enrollment. Common DTP segments in an 834 include the benefits coverage effective date (often with a qualifier like 348 = Benefit Begin Date) and possibly an end date (349 = Benefit End Date) if the transaction is terminating coverage or indicating an end of eligibility. Dates are formatted as CCYYMMDD. For example, DTP348D8*20250101~ means coverage effective date of 2025-01-01.
SE – Transaction Set Trailer: Marks the end of the individual 834 transaction and contains a segment count for that transaction for validation.
GE – Functional Group Trailer: Marks the end of the group of 834 transactions (if multiple were in one file) and includes a count of how many transaction sets were included.
IEA – Interchange Control Trailer: Closes out the interchange, providing a count of the functional groups and a final control number check.
The above segments and loops ensure that an 834 file is both comprehensive and unambiguous, but it can look quite cryptic at first glance. Here is a simple example of a snippet from an EDI 834 file, using a fictional company Daily Planet (Plan Sponsor) and an employee, Clark Kent, enrolling in a health plan:
[[Note]]
ISA*00*.........*ZZ*DAILYPLANETID*ZZ*METROPOLISHLTH*250819*1618*^*00501*000000123*0*T*:~
GS*BE*DAILYPLANET*METROPOLISHLTH*20250819*1618*1*X*005010X220A1~
ST*834*0001~
BGN*00*12345*20250819*1618*ET*4~
N1*P5*Daily Planet*FI*123456789~
N1*IN*Metropolis Health Insurer*FI*987654321~
INS*Y*18*030*XN*A*E**N*Y*Y~
REF*0F*CLARKKENT001~
REF*1L*DP-001~
NM1*IL*1*KENT*CLARK*T***34*999887777~
N3*344 CLINTON ST*STE 100~
N4*METROPOLIS*NY*10001~
DMG*D8*19800101*M~
HD*030**HLT*PLAN123*EMP~
DTP*348*D8*20250101~
DTP*349*D8*99991231~
SE*15*0001~
GE*1*1~
IEA*1*000000123~
[[/Note]]
In this example, the file headers (ISA/GS) are shown with placeholder IDs for the sender and receiver. The BGN segment indicates this is batch number 12345 created on 2025-08-19. The N1*P5 segment names “Daily Planet” as the plan sponsor (with a fictional federal ID 123456789), and N1*IN names “Metropolis Health Insurer” as the insurance carrier (ID 987654321).
The INS segment with Y*18*030 indicates an active subscriber record (Y = active, 18 = self (subscriber), 030 = enrollment maintenance code for “addition or change”) and some other flags. Two REF segments provide reference IDs: one (0F) is a subscriber identifier CLARKKENT001 and another (1L) might be a group or policy number DP-001. The NM1*IL segment gives the subscriber’s name, Clark T. Kent, and uses 34 to denote that the following number is an SSN (here 999887777 as a dummy SSN). The address is listed in N3/N4 as “344 Clinton St, Suite 100, Metropolis, NY 10001”.
The DMG segment shows Clark’s date of birth (1980-01-01) and gender (Male). The HD segment indicates the type of coverage – here “HLT” (health) with a plan code “PLAN123” and an coverage level “EMP” (perhaps Employee-only coverage). Finally, DTP348 gives the coverage effective date of 2025-01-01, and DTP349 (if present) could indicate an end date (here 9999-12-31 is often used as a placeholder end date meaning “open-ended” coverage). The transaction is closed with the SE segment, and the file is closed with GE and IEA.
Real-world 834 files can be much longer and include multiple INS loops – one for each subscriber, followed by loops for their dependents (each dependent would have INS with relationship code like 19 for spouse or 01 for child, etc., plus their own NM1, DMG, etc.). The structure and codes can also vary slightly based on each insurance carrier’s specific companion guide (for instance, some carriers might expect certain REF codes or additional segments). Nonetheless, the core layout remains as illustrated above.
Implementing an EDI 834 Interface: Team and Timeline
Setting up an EDI 834 enrollment feed is a project that typically involves both business and technical stakeholders. It’s not just an IT project – it requires understanding of benefits data and coordination with external partners (the carriers or EDI vendors). Here are key considerations for implementation:
- Cross-Functional Team: Assemble an internal team that includes benefits/HR personnel, who understand the enrollment rules and data; accounting/finance staff, who may use the data for billing reconciliation; and IT/EDI specialists, who handle the technical mapping and connectivity. This mix ensures that when decisions arise (like how a particular plan code should be represented, or how to handle specific business rules), the right experts are involved. Each insurance carrier will usually provide an EDI companion guide (sometimes called an EDI “structure” document) describing exactly how they implement the 834 format. Your team will need to review this guide in detail to configure your output file to the carrier’s specifications.
- Mapping and Development: The IT/EDI specialist (or EDI software) must map data from your source system (e.g., HRIS or benefits administration system) into the 834 format according to the carrier’s requirements. This includes mapping your internal fields (like employee ID, plan selections, dependent info) to the appropriate segments and elements in the 834. Often this involves using an EDI translator or middleware that can be configured with the rules. If you’re using a third-party EDI 834 or software like Tabulera’s EDI 834 Module, they might handle much of this mapping for you once you provide them the data specifications.
- Testing with Carriers: Testing is crucial before an 834 feed goes live. Typically, you will exchange test files with the insurance carrier’s EDI team. They will validate that the file is formatted correctly and that their system can ingest it. This often uncovers issues like mismatched codes or missing required data, which need to be corrected. Only after you pass the carrier’s test scenarios (which may include cases for adding new enrollments, making changes, and terminating coverage) will the carrier approve moving to production. This testing phase ensures that when you send real enrollment data, it will update the carrier’s system without errors.
- Timeline: The time it takes to implement an EDI 834 interface can vary widely. It depends on factors such as the carrier’s responsiveness, the complexity of your plans, and the availability of resources. Generally, the analysis of the carrier’s EDI requirements, building the file, and end-to-end testing can take anywhere from a few weeks to a few months. Industry experience shows a range around 3 to 12 weeks for a typical 834 implementation project, from project kickoff to go-live. More straightforward cases (single plan, using a modern EDI platform) might be on the shorter end, whereas complex scenarios (multiple carriers, custom business rules) lean toward the longer end. Tabulera gets the EDI files live in 30 days.
- Resource Considerations: During implementation, your team will need to dedicate time to meetings with the carrier (or EDI vendor), data mapping exercises, and iterative tests. Make sure to budget sufficient time for your IT staff to work on file development and for your benefits staff to validate that the enrollment information is being transmitted correctly (e.g., verifying that enrollments in your HR system match what appears in the carrier’s test system after they process the 834). The process often involves a lot of back-and-forth communication to get everything “just right,” so patience and attention to detail are important.
One thing to keep in mind is that each insurance carrier has its own nuances. If you are implementing 834 feeds for multiple carriers, you will repeat this process for each one, since each carrier’s companion guide might differ slightly (different required fields, different code values allowed, etc.). However, once the initial setup is done and working, adding new hires or changes via EDI becomes much less labor-intensive than manual entry.
Ongoing EDI 834 Exchange: Cadence, Monitoring, and Maintenance
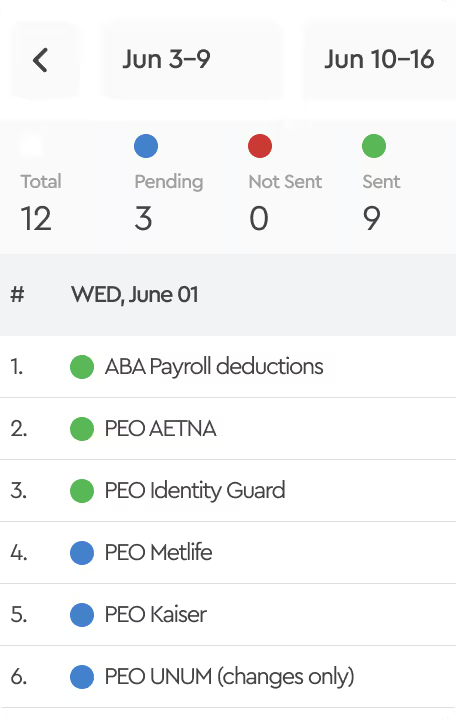
Once your EDI 834 feed is live, using it becomes a routine part of your benefits administration process. Typically, companies will send enrollment update files on a regular cadence (schedule). Common schedules are weekly transmissions (e.g., every Friday) or per payroll period, so that any HR changes (new enrollments, terminations, etc.) from that week are sent in batch to the carrier. Some may send files daily if volume is high or if needing near-real-time updates (for example, some systems can trigger an 834 file generation whenever a change is made). The schedule is usually agreed upon with the carrier in advance.
Files are usually transmitted through secure channels – often via SFTP (Secure FTP) or another secure file transfer service – to protect the sensitive personal health information contained in the 834 (since these files have names, SSNs or IDs, birthdates, etc., they must be handled in a HIPAA-compliant manner). The transfer process can be automated so that files are sent and received without manual intervention. For instance, your system might drop an 834 file to a secure folder every Friday, and the carrier’s system automatically picks it up for processing.
Monitoring acknowledgments: As mentioned earlier, you should expect a 999 acknowledgment in return for each file, usually within minutes or a day of the file delivery (depending on the carrier’s system). It’s important to check these 999 responses. An accepted 999 means the file structurally passed; a rejected 999 means nothing was processed – you’d need to fix the error (e.g., maybe an invalid date format or a missing required segment) and resend. Having alerts or notifications for failed acknowledgments is a good practice.
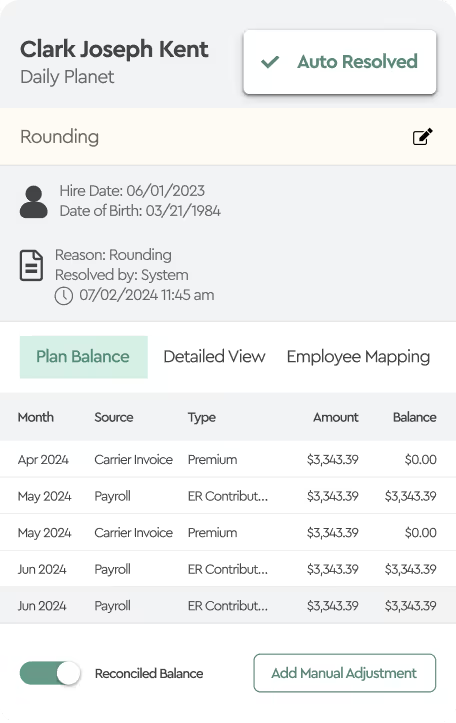
Discrepancy reports: In many cases, after processing the file, the carrier may provide a response report or error/discrepancy report that details any enrollment records from your 834 that could not be applied. For example, if one of the records in the 834 had a problem (like a dependent listed without a date of birth, or an employee not found in the carrier’s system), the carrier’s system might accept the file but note those issues on a report. It’s typically the responsibility of the sending entity (your team or your EDI vendor) to review these discrepancy reports each time and resolve any issues. Resolving issues might involve correcting data in your HR system (and then that correction will flow in the next 834 file) or manually informing the carrier of adjustments if needed.
It’s important to assign an owner for this ongoing process. Usually, the benefits or HR team will be the ones who understand the data and can fix it. They should know how to read the carrier’s report or have a tool to interpret it, since it often references members by IDs or error codes. Maintaining this process diligently is imperative to keep everything in sync – coverage accuracy depends on continuously addressing any errors that come up. If errors are left unresolved, an employee might think they’re enrolled when the carrier actually didn’t activate their coverage, leading to unpleasant surprises at the doctor’s office. Thus, having controls in place (like a checklist to verify each weekly file was sent and accepted, and each discrepancy report was reviewed) will ensure the EDI feed continues to deliver value.
Changes and updates: Over time, you may need to update your 834 feed. Perhaps you add a new benefit plan (which means new codes to send), or your company changes payroll/HR systems, or the carrier updates their companion guide for a new version of the standard. EDI 834 is not “set and forget” – it may require periodic maintenance. Upgrading from one version to another (like from 5010 to future versions) could be a project with the carrier. Always communicate with carriers if you plan changes on your side that could affect the file (for example, if you’ll start sending new deduction codes or if you acquire another company and suddenly have a spike in enrollments).
Reading and Troubleshooting EDI 834 Files
For IT professionals familiar with EDI, an 834 file is straightforward to parse with the right tools or EDI software. However, for benefits administrators or others who are not EDI experts, the file’s raw format is hard to read. Each segment code and cryptic value needs interpretation. So how do you “read” an EDI 834 if you need to verify something?
Understanding the structure: If you open an 834 file in a text editor, you’ll see the segments separated by tildes (~). The first thing is to identify the sections. Look for the ISA and GS at the top – these tell you the sender/receiver and that you indeed have the right file (834). Next, find the ST*834 segment which marks the start of the actual enrollment data transaction. Everything between ST and the matching SE is one complete 834 transaction set. If multiple ST...SE segments exist, there are multiple transactions in one file (which is less common for enrollment files – usually it’s one transaction listing multiple members).
Key segments to review: Within the transaction, you’ll want to pinpoint certain segments for the information you need. The BGN segment can tell you the batch number or purpose of the file (for example, some might use a code to indicate if it’s an initial load vs. ongoing maintenance). The INS segments mark each member record, so scanning for "INSY" or "INSN" helps you locate the start of each person’s data. The INS will also tell you if that person is a subscriber or dependent (relationship code) and if the record is adding, changing, or terminating coverage (maintenance type code). Right after an INS, you should see that person’s NM1 (Name) segment and associated details like REF (IDs) and DTP (dates). By reading the NM1 and related segments, you can extract the member’s name, their identifying numbers, coverage effective dates, etc.. For instance, to find if a specific employee (say John Doe) was included in the file, you might search the text for "DOE*JOHN" which would appear in the NM1 segment for that person.
Extracting specific data: If you are looking for a particular detail, such as the effective date of coverage for an employee, you would navigate to that employee’s INS loop and find the DTP segment with qualifier 348 (Benefit Begin Date) within that loop. Or if you need to verify what plan they were enrolled in, find the HD segment in their record which might contain the plan code. Addresses will be in N3/N4 following the NM1 if present.
Checking file integrity: Toward the bottom of the file, verify the SE segment count matches the actual number of segments in the transaction and that the GE and IEA control numbers match the ISA/GS. This is more of a technical check, but it ensures the file isn’t truncated or missing segments. An issue in these can indicate the file was incomplete.
Tools for easier reading: Because manually reading raw EDI is tedious and prone to misinterpretation, many organizations use EDI parser tools or have their EDI vendor provide a human-readable version of the 834.
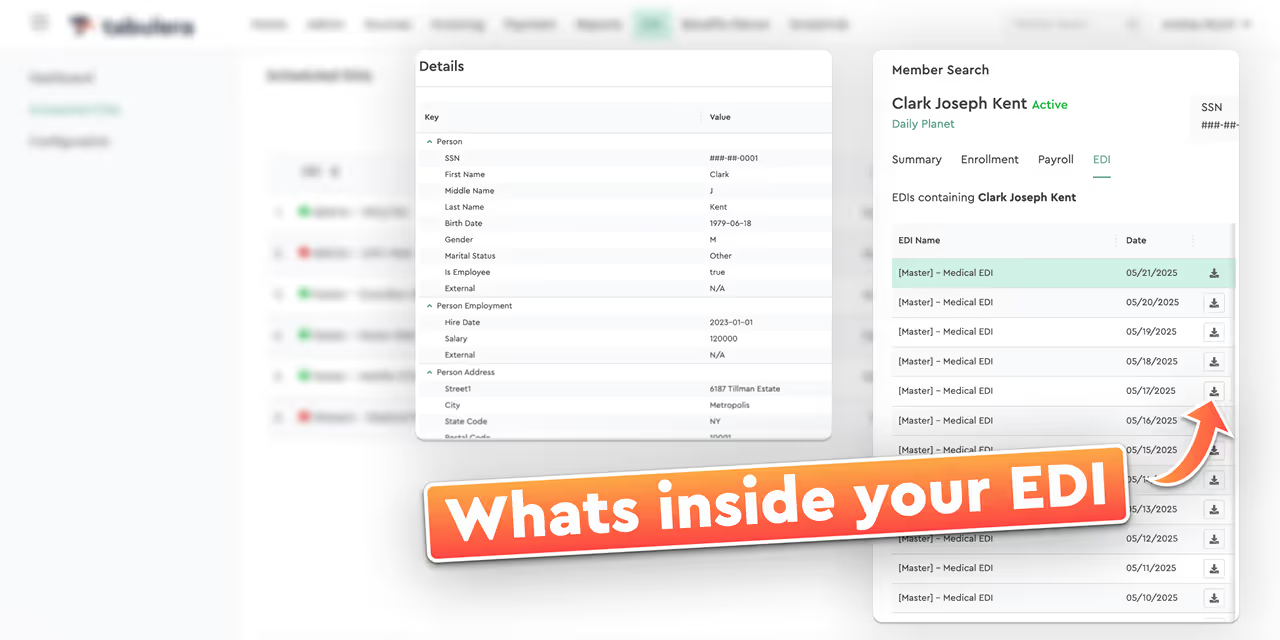
For example, some tools can convert the 834 into a CSV or a nicely formatted report listing each member and their data fields. In our case, we’ve introduced a feature called Member Search that translates EDI 834 files into easily understandable data, allowing even non-technical users (like brokers, call centers or HR teams) to quickly look up an employee or dependent and see their enrollment info without sifting through raw EDI lines. This kind of tool can answer questions like “Is this employee’s new enrollments in the latest file?” or “What dependents were included for this employee?” by simply searching for the member’s name or ID. Member Search essentially parses the EDI behind the scenes and presents the relevant information in plain language, which is a huge time-saver for benefits teams who need quick answers from the EDI feed.
If you don’t have an automated tool, another strategy is to refer to the carrier’s companion guide while inspecting the file – the guide will define each segment and element so you can decode what each line means. Over time, as you become familiar with the 834 structure, you’ll get better at eyeballing common segments and understanding them.
Benefits of Using EDI 834 for Enrollment
Implementing EDI 834 for benefits enrollment can require effort up front, but the payoff is significant. Key advantages include:
- Efficiency and Speed: EDI automates the transfer of enrollment data that would otherwise be entered manually. This cuts down on the repetitive data entry work of logging into carrier websites and typing in each new hire or change. A properly functioning 834 feed means that when you update your HR system, those updates are compiled and sent out automatically. The result is faster updates to coverage – employees get enrolled or changes processed in days instead of weeks.
- Reduced Errors: Manual data entry is error-prone – typos or missed fields can lead to coverage mistakes. The 834 file format minimizes these errors by taking data directly from your source system and standardizing it. While errors can still occur (for example, if the source data is wrong), there’s no risk of human transcription mistakes during submission. Additionally, the structured format validates the data (e.g., a date field will clearly show if a date is missing or misformatted, triggering a correction before it loads). Overall data accuracy improves, leading to fewer discrepancies between your records and the carrier’s records.
- Consistency and Compliance: Because the 834 is a national standard, it enforces a level of consistency in how enrollment data is communicated. This helps ensure compliance with regulations (HIPAA, ACA reporting requirements, etc.) since you’re using the approved format for data exchange. It also means if you switch to a new carrier or benefits administrator, they will likely accept the same 834 format, making transitions smoother.
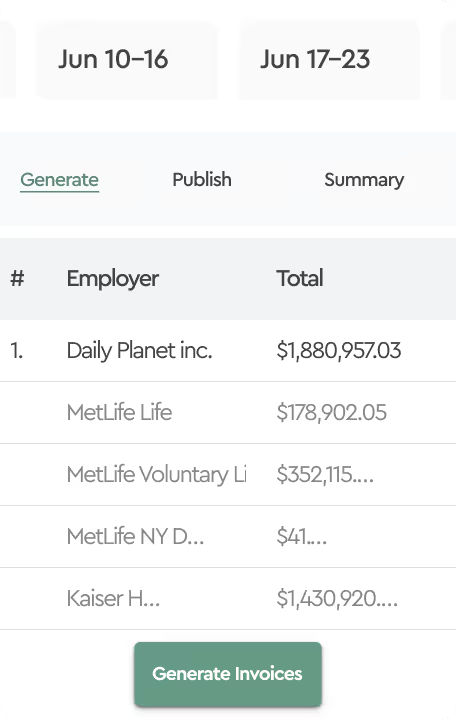
- Rich Data and Custom Fields: The 834 format isn’t limited to just the basics of enrollment; it allows transmission of a variety of data elements. For example, you can include departmental codes, division identifiers, or job class info in the 834 (often via REF segments or other optional fields). These additional fields can later show up on your carrier’s premium invoices or reports. That means you can get more detailed billing breakdowns (e.g., premiums by department) without manual effort, simplifying accounting reconciliation.
- Improved Employee Experience: When enrollments are processed quickly and accurately, employees experience fewer issues like missed coverages or ID card delays. There are fewer panicked calls from employees at a pharmacy saying “My insurance isn’t active.” This improved reliability leads to fewer employee complaints about benefits. Also, your benefits team shifts from tedious form-filling to an oversight role – they spend time on verification and exception handling rather than typing data. This elevates their job satisfaction and lets them focus on higher-value tasks like analyzing benefits utilization or improving communication, instead of being stuck in data entry mode.
- Scalability: As your organization grows, the volume of enrollment changes grows too. An electronic process scales far better than a manual one. Whether you’re adding 10 new hires or 1,000 new hires, the 834 file process is largely the same automated flow. This scalability is crucial for fast-growing companies or those that experience seasonal enrollment spikes. It also becomes indispensable if your company goes through mergers or adds new groups – instead of overwhelming your benefits staff with administrative work, the EDI can handle the surge as long as the data is fed into it.
In summary, using EDI 834 drives efficiency, accuracy, and timeliness in benefits administration. It aligns with the digital transformation of HR processes – moving away from paper forms and isolated systems toward integrated data exchange. When combined with proper controls and monitoring, an 834 feed significantly reduces the administrative burden and the risk of coverage errors.
Challenges and Best Practices
While the benefits are clear, it’s also important to acknowledge challenges and share some best practices when handling EDI 834 files:
- Data Readiness: EDI will only send what data you have. One common challenge is ensuring your HR system or enrollment platform has all the required information to populate the 834 file. Missing data (like a missing date of birth or SSN for a dependent) can cause rejections. Best practice is to enforce required fields in your source system and run data audits before sending the file. For example, run a report of all employees with missing key fields prior to go-live.
- Carrier Variations: Each trading partner might have slight differences in how they implement the 834. One insurer might require a value that another does not. Maintain a mapping documentation for each carrier’s feed that notes these specifics. This becomes vital for troubleshooting issues because you can refer back to what each carrier expects. If possible, use a flexible EDI solution that allows you to handle variations through configuration rather than hard-coding, so updates are easier.
- Testing Changes: Whenever you or the carrier makes a change (for instance, you add a new field to the 834, or the carrier updates their system), conduct regression testing. Send test files and have the carrier confirm all is well. Do not assume that a change is minor; even a small tweak can have unintended effects on file processing.
- Monitoring and Alerts: Establish a monitoring mechanism for your EDI process. This could be as simple as an automated email confirming file sent and 999 received, or as robust as an EDI dashboard that flags errors. The key is, you want to know if something goes wrong before it becomes a big problem. For instance, if a weekly file fails to send, an alert should notify IT to resend it or fix the issue immediately, rather than discovering a month later that a batch of enrollments never went through.
- Security: Always send EDI 834 files securely. Use encryption (PGP encryption on the file, for example) if required in addition to secure channels. Ensure that only authorized personnel have access to these files, as they contain protected health information. Work with your IT security team to include EDI in your data protection policies.
- Backup Processes: Have a contingency plan in case the EDI process encounters a prolonged issue. For example, if your EDI system is down or a critical error is preventing file transmission for a few cycles, you might need to fall back to manual entry on the carrier’s portal as a temporary stop-gap. Knowing how you will handle that scenario (and how to catch the carrier data up with a big file later) will save stress if it ever happens.
By being mindful of these challenges and proactive with best practices, you can ensure your EDI 834 integrations run smoothly and continue delivering value over the long term.
How to Cut EDI 834 Implementation Time to Just 30 Days
One of the biggest struggles with EDI 834 is simply getting files live. In the industry, even a basic setup—one HRIS or payroll system connected to one carrier—often takes 3 to 6 months. When multiple feeds are involved, it can drag on for a year or more. Some organizations even spend close to two years trying to implement a single file before finally seeking outside help.
Working with the right EDI 834 vendor changes that experience. Tabulera gets EDI 834 files live in about 30 days, helping employers, brokers, and outsourcers avoid long delays and stalled projects. Beyond implementation speed, the EDI Connectivity Module provides transaction tracking, scheduling, and Member Search to make ongoing file management and troubleshooting easier.