July 2, 2024
Benefits Invoice Audit: Helping Brokers Support Their Clients
Why Are Benefit Invoice Audits Important for Brokers and Their Clients?
Employers audit their employee benefit invoices to catch errors and correct discrepancies, ensuring proper financial controls and making sure employees receive the health coverage they selected. In benefits administration, errors and discrepancies often arise from human mistakes on both the carrier and employer sides. Common issues include:
- System Misconfiguration: Incorrect rates being applied, wrong eligibility dates etc.
- Terminated Employees on Invoices: Employees who have left the company but are still being billed cause unnecessary expenses.
- New Hires Not Appearing on Invoices: New hires missing from invoices can lead to compliance issues.
Implementing benefit invoice audit processes helps identify and correct issues promptly, maintaining financial accuracy and efficiency. Brokers can assist their clients by leveraging tools and expertise to streamline this audit process, ensuring accurate billing.
Two Ways Brokers Can Help Their Clients with Benefit Audits Using Tabulera:
1. Benefit Invoice Audits As A Service.
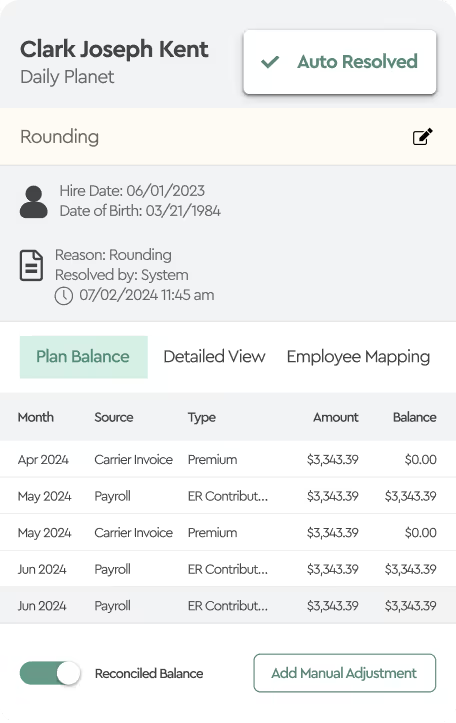
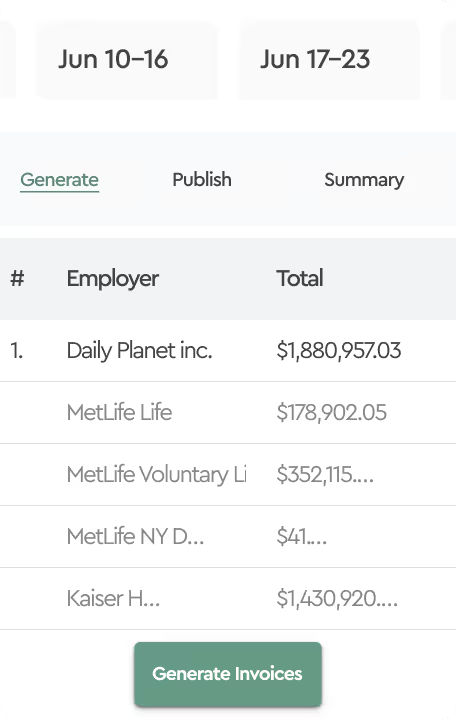
Brokers can leverage Tabulera’s Benefits Reconciliation Module by integrating it directly with any HR and Benefit Enrollment platforms. This integration allows brokers to upload clients’ carrier invoices into Tabulera, which then automates the discrepancy identification process.
According to our research, the efficiency of automated matching is around 84% with Version 3.0 of the Benefits Reconciliation Module; meaning brokers need to manually review only 16% of the total benefits-eligible employee population. Of these, statistically 10% are new hires and terminations in transit, which should auto-resolve next month, while 6% will have actual rate discrepancies, system misconfigurations, or plan mismatches that can cause financial leakage for the employer.
- Automation: The system automatically matches invoices with enrollment data, significantly reducing manual effort. It efficiently identifies enrollments in transit (such as employees hired after the invoice generation date) and terminations in transit (employees terminated after the invoice generation date), as well as plan mismatches. The system highlights all discrepancies in order to address system misconfigurations or data errors.
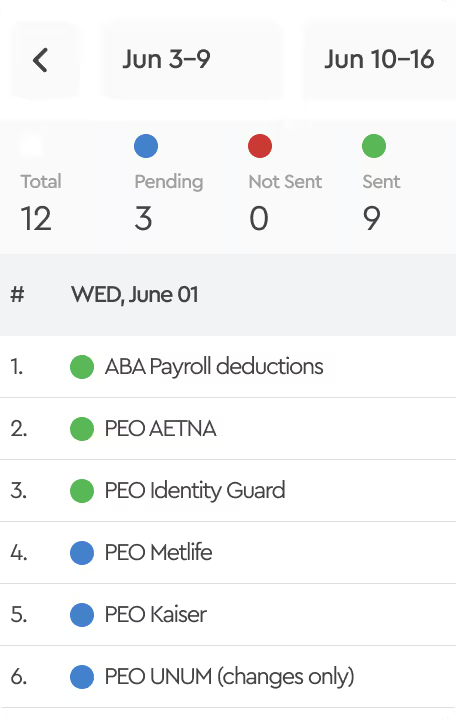
- Efficiency: Brokers can reconcile all of their clients' invoices or select specific clients that need this service within a single platform, streamlining their operations and enhancing service delivery.
2. Referrals for Enterprise Accounts.
Some brokers, particularly smaller ones, manage large, complex accounts that require detailed payroll reconciliations. For these accounts, brokers can become a referral source, directing clients to Tabulera’s solutions. This approach is especially beneficial for brokers who lack the capacity to provide detailed reconciliations effectively. By offering Tabulera’s software, brokers can equip their clients' HR teams with the necessary tools to perform benefits reconciliation accurately on their own, retaining their large clients and demonstrating creativity in finding solutions to their problems.
- Cost Savings: The reduction in billing errors and write-offs leads to significant cost savings for employers.
- Financial Control: Controllers and CFOs will appreciate the improved financial oversight, knowing that their benefit plans are frequently reconciled.
Benefits of Using Tabulera’s Software

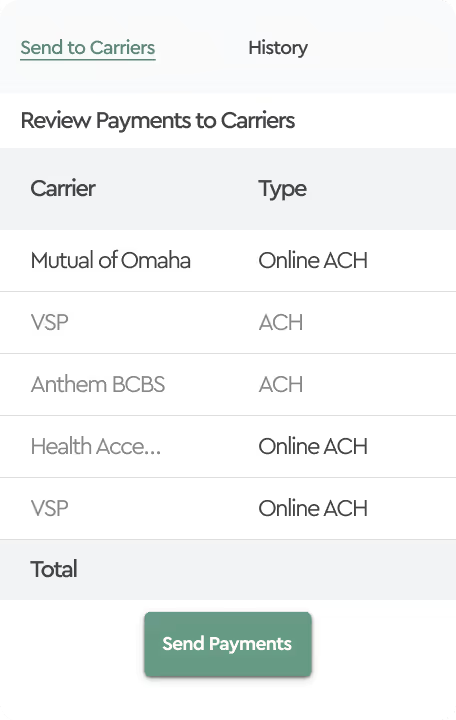
Tabulera’s Benefits Reconciliation Module is highly effective for accurately and efficiently auditing list-bill or self-bill invoices against enrollment or payroll data. The platform focuses on verifying that charges from insurance carriers or self-bill calculations align with actual enrollments and payroll deductions.
Key benefits include:
- Monthly Premium Reconciliation: Ensures that the premiums billed by carriers accurately reflect the enrolled employees and their selected plans, reducing overpayments and billing errors.
- Reporting: Provides detailed reports that highlight discrepancies, allowing brokers to address issues with carriers promptly and ensure accurate billing.
- Enhanced Efficiency: Tabulera’s software automates the tedious task of matching carrier premium invoices with payroll and enrollment data. This automation not only reduces the chances of manual errors but also ensures that discrepancies are identified and addressed promptly.
- ROI: Our clients have experienced significant financial benefits from using Tabulera’s software. For example, one case study revealed that a client eliminated 97% of benefit write-offs, showcasing the substantial ROI and improved financial accuracy achieved through our platform.
- Seamless Integration: Tabulera’s Benefits Reconciliation Module accepts enrollment and payroll data via API, reports, and SFTP connections from the most popular HR and Benefits platforms such as Employee Navigator, Workday, UKG Kronos, and ADP. It can also accept any enrollment or payroll report in Excel or CSV format. This compatibility ensures that brokers can easily incorporate our solution into their clients' existing systems without disruption.
Conclusion
By utilizing Tabulera’s Benefits Reconciliation Module, brokers can offer enhanced services to their clients, ensuring accurate and efficient benefit invoice audits. Whether integrating our module into their own systems or referring larger clients to us, brokers can trust Tabulera to deliver reliable, automated solutions that drive productivity and financial accuracy. Our proven technology not only simplifies the reconciliation process but also provides significant ROI, making it an essential tool for modern benefits administration.