






What is Benefits Reconciliation?
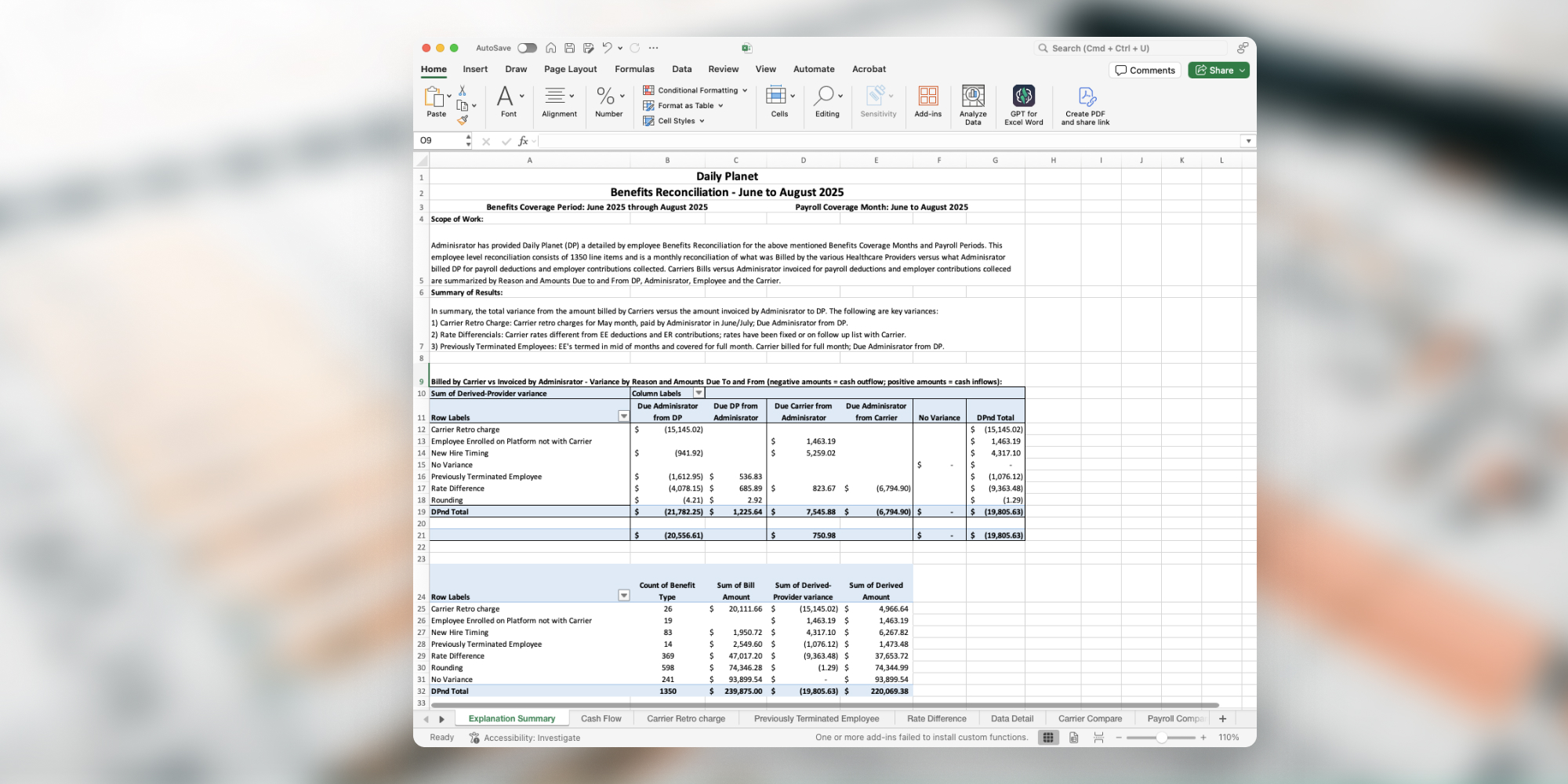
, also called - is the monthly process of comparing carrier invoices against payroll and enrollment records.
The goal is simple - make sure every employee is billed correctly
Without reconciliation, billing errors slip through - from premiums still charged for terminated employees to missed refunds after carrier deadlines, and even active employees losing coverage.
Regular reconciliation stops premium leakage, protecting both your budget and your people.
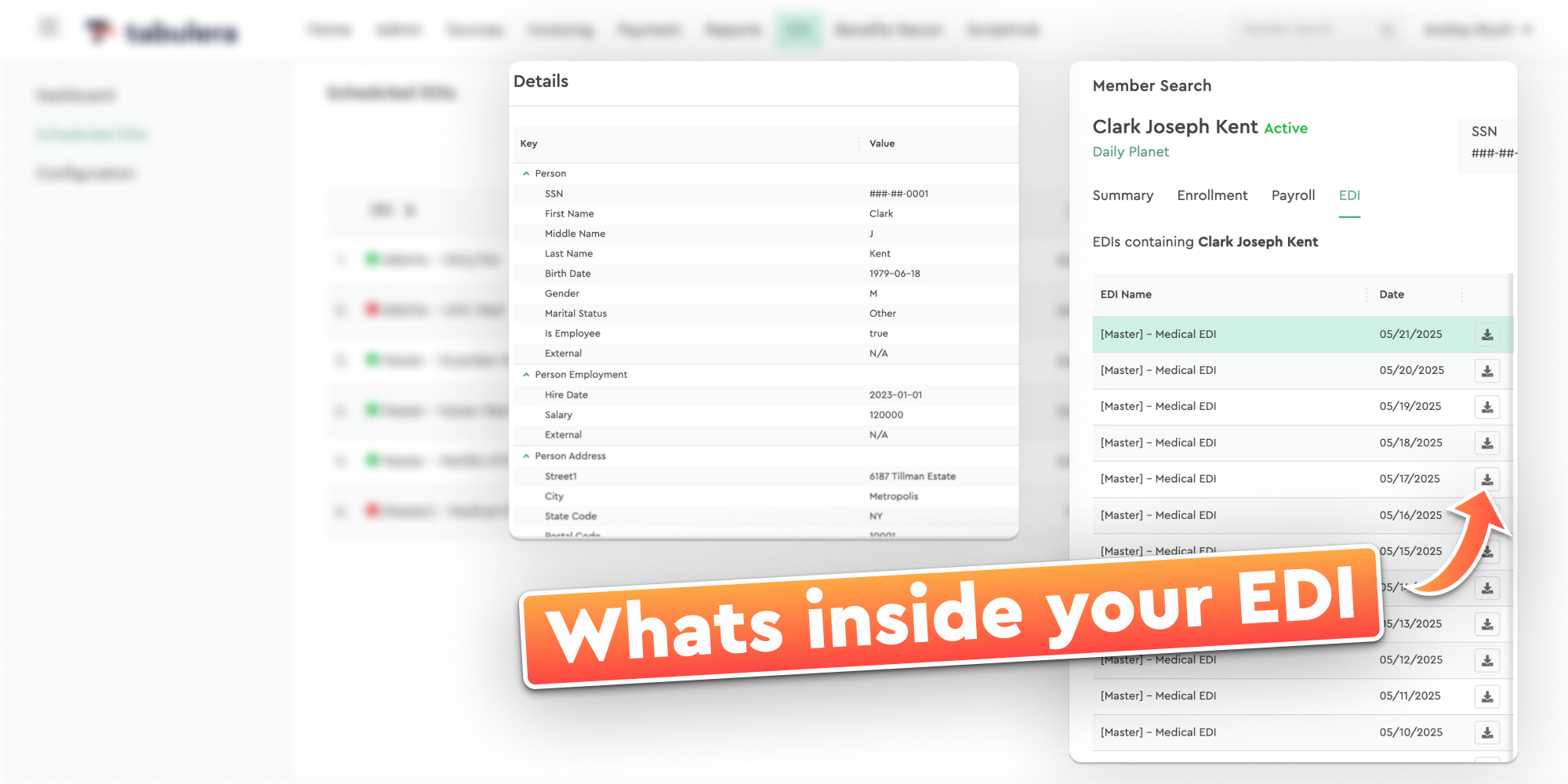
Meet Tabulera's Benefits Reconciliation Module
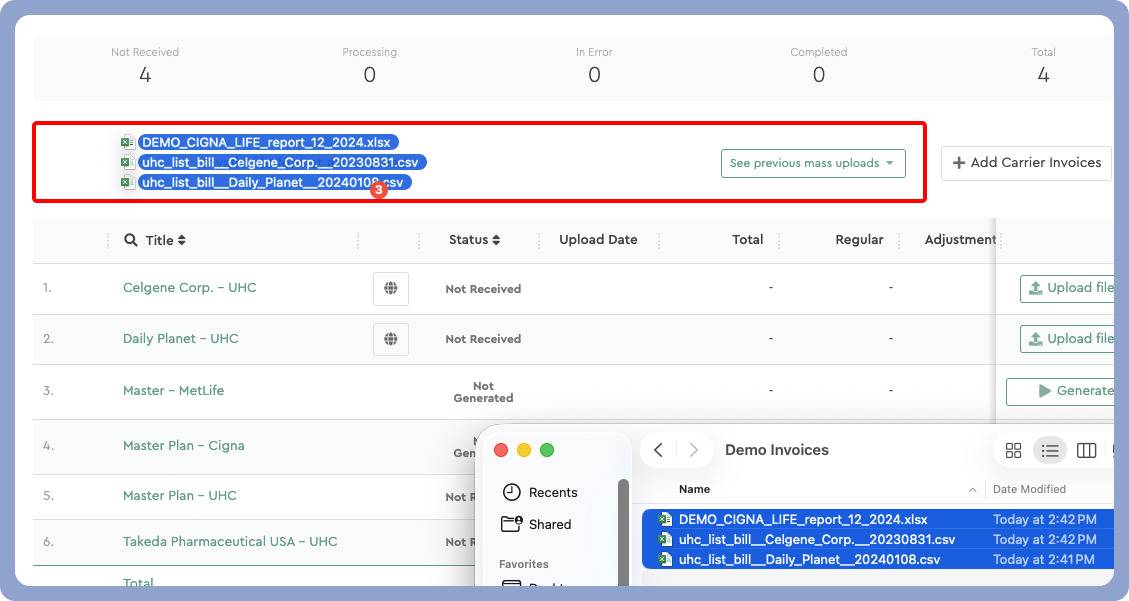
Tabulera is the first easy-to-use tool built for employers, PEOs, and outsourcers to catch benefit billing errors faster, reduce manual work, and stay compliant.
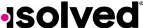
Simply upload your source files - from any HRIS, Payroll, or COBRA system - along with your carrier invoices. Tabulera will filter out employees with no issues, flag discrepancies, and categorize them so you can quickly find the root cause and fix it.
Benefit teams use Tabulera to:
Follow an easy, repeatable process
Automatically filter out employees without issues
View all source data in one place - and trace issues back to HRIS/Payroll systems or the carrier
Leave notes and color tag variances
Generate reconciliation reports for your finance team
Excel was never built for Benefits Reconciliation
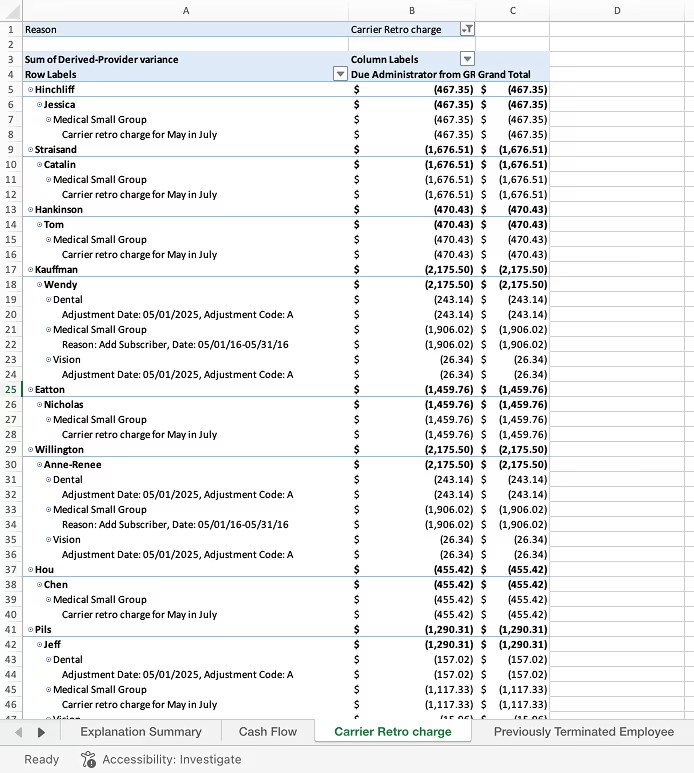
For years, benefits reconciliation has meant juggling spreadsheets, tabs, and pivot tables – often in a workbook built by one person with no documentation and no way to track cumulative plan balances.
Even the best Excel reconciliation setups are hard to audit, easy to break, and nearly impossible to scale. Everyone hopes to find the perfect Excel reconciliation template, but the reality is that Excel simply wasn’t designed to handle the complexity and volume of modern benefit invoice audits.
Common pitfalls of reconciling in Excel:
Reconciliation template built by one person
Most Excel workflows rely on a single expert—if they leave, the process breaks.
Manual and error-prone
Copy-pasting from invoices, payroll, and enrollment systems takes hours and invites mistakes due to inconsistent employee info.
Hard to track over time
No clean way to manage monthly changes, prior adjustments, or audit history.
No audit trail
Changes happen silently. No version control, no accountability, no compliance confidence.